All three Drs. Mollner take pride in constant continuing education. We continue to study the newest methods and techniques in dentistry on a regular basis. This allows us to perform the most proven, trusted, and cutting edge dentistry in the world. Through our studies, we occasionally find research we think our patients would be interested to know. Posted below you will find our breakdowns of the newest studies, techniques, and findings and how they are influencing our practice and your oral health.
Got a question you think others might also want to know? Anything dentistry related, big or small…like, What is a crown? Why do we have to brush our teeth? How do cavities work? Go ahead…
Leave your question in the comments section below and we may publish your question with one of the doctor’s answer.
June 7 2013 Treatment of Sensitive Gum-line Fillings – Dr. Ben
Often times, patients come to my office with sensitive areas along the gum line of their teeth. These sensitive areas are usually caused by the patient brushing too aggressively to the point of slowly scrubbing away protective gum tissue and tooth structure. They can be worsened in patients who grind their teeth (heavy grinding can cause slight flexure of the enamel which is very similar to glass and breaks when it is flexed). These exposed areas are more susceptible to cavities, but can be very sensitive even in the absence of a decay. Treatment options typically include covering the affected area with a thin, permanent tooth-colored filling material or applying desensitizing paste (potassium nitrate). In a new study published in the Journal of American Dental Associatioin (JADA 2013: 144(5):495-506, both treatments showed improved symptoms of sensitivity in groups of people, but the group that had permanent filling material placed showed a significantly higher reduction in sensitivity than the group with desensitizing paste.
The bottom line? We offer both type of treatments in our office, and if you have sensitive gum-line fillings we can help. Placing a thin filling over the affected area usually works better, protects the exposed area for years to come, and is covered by most dental insurances.
Clinically, I have always seen better results with filling material vs. desensitizing pastes, but it is nice to see peer-reviewed research supporting this.
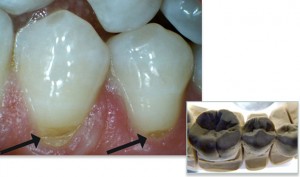
Arrows show cervical lesions (gum line cavities) on lower pre-molars before treatment.
Nov 3, 2011 – Dr. Ben
On my radar:
This morning I read a research article about improved bonding of white fillings (composite) to tooth structure. Generally speaking, teeth are made of two types of hard tissue: enamel and dentin. Enamel is the hard outer coating that protects the tooth, and dentin is the softer inner part of the tooth that is sensitive when having a filling done. Bonding a white filling to enamel is very predictable and long lasting, however bonding to dentin is a much weaker bond. Unfortunately, most fillings have decay into the dentin where at least part of the filing will have to be bonded to dentin. The current average filling bond to dentin lasts only 5.7 years. This new research shows that an enzyme that is naturally occuring in the dentin is responsible for the weak bond strength, and the enzyme is activated by acid given off by bacteria (the stuff causing the tooth decay!) It is nearly impossible to kill all bacteria inside of a filling because they can live inside the pores of the tooth and they also live by the millions in your saliva. It is safe to seal a small amount of them inside the filling because their food source is sealed off and they will die, but not before emitting enough acid to activate the enzymes which weaken the bonded filling. The study shows that a chemical called Chlorahexadine (CHX) can kill bacteria and block the enzyme that weakens the dentin bond. The bottom line: Using adhesives with CHX may increase bond strength and raise the dentin bond beyond the average 5.7 years. Currently no dental companies offer such an adhesive, but after the publication of this study I will be monitoring them for the addition of CHX, and plan on testing this adhesive when it is available.
November 9, 2011 – Dr. Rena
Last night I attended a dental society meeting discussing Implants for patients who have lost all of their teeth. The latest technique is called “All on 4” which is basically 4 upper implants and 4 lower implants and an upper and lower denture attached to these implants. The stability is similar if not stronger than natural teeth and looks very natural. This concept allows a patient with no teeth to have a full set of permanent teeth that can chew even the toughest of foods within 3 months, and only a small number of implants in order to save cost for the patient. We currently have everything necessary to perform this type of treatment from start to finish in our office right now!
December 19, 2011 – Dr. Ben
There are currently recommendations by the American Academy of Orthopedic Surgeons that any patient who has had a joint replacement take an antibiotic before invasive dental procedures. The concern is that bacteria in your mouth can be forced into your bloodstream and cause an infection in the artificial joint. Normally your body’s immune system will kill this small amount of bacteria within a few hours, however, people with artificial joints have a weakened immune system surrounding the joint, and bacteria can actually cause an infection and ultimately cause the artificial joint to be rejected by your body.
I reviewed a new research paper this morning that studied people with artificial joint rejections and the relationship to invasive dental work. The study showed that there was no significant association between joint rejection and invasive dental work.
What does this mean for my patients? I will continue to recommend antibiotics to my patients with artificial joints as a safety precaution. I would rather err on the safe side to prevent a major complication, but it is good news for patients that dental procedures are less likely to cause joint infections than previously thought. In the worst case scenario (antibiotics are forgotten, mistimed, or underdosed) the patient is not likely to have complications anyway.
September 3, 2012 – Dr. Ben
Many patients ask me about the move from amalgam (silver) fillings to composite (white) fillings and the harms associated with silver amalgam (more on this subject later). But what many people don’t think about, are the health factors associated with composite fillings. Probably the main chemical concern with composite fillings is the inclusion of BPA. This is the same concern as you see in plastic food containers, and many of the nalgene-style water bottles now carrying BPA-free labels.
BPA (Bisphenol A) is a molecule used to make many types of plastics (there is some plastic in white fillings). It is concerning because studies show BPA can act as a hormone mimetic (a copy of a hormone, which can signal hormone pathways in the human body).
In 2011, we discontinued using composite filling materials that contain BPA. There are several alternatives, one of which we had already been using even before we knew as much about BPA. The BPA-free composites show equal or superior wear quality to those with BPA, and the esthetics of these modern composites look unbelievably like real enamel.